Case studies
Case Study #1
Joe Smith with early onset Cataracts and early AMD.
Joe is a 60 year-old Accountant who relies on either the car or train travel to get to the Melbourne CBD every day from Geelong.
Joe is moderately short-sighted and has recently noticed more glare from the headlights when driving at night.
His eye doctor diagnosed him with early onset cataract and AMD (Age-Related Macular Degeneration).
As Joe’s cataract (cloudy lens) was not too far advanced, his eye doctor advised him that is vision was still good enough for driving. It was the debilitating glare from oncoming headlights, however, which caused Joe much grief on his long trips. Joe’s very early AMD has only interfered with his ability to read poorer contrast print, such as that in newspapers.
An Orthoptic Low Vision Assessment was recommended at this early stage, so that Joe could explore glare control and lighting, plus be made aware of his future options, should his vision become worse.
Using a Lux Metre, the Orthoptist was able to assess the level of lighting in Joe’s office and reading room at home, making relevant recommendations in accordance with Standards Australia. Appropriate task-lighting was recommended and supplied. Illuminated hand-held magnifiers were also explored for future reference. In addition to this, sunglasses for UV protection and glare control during the day and night were explored.
Joe received further information regarding the usual progressive nature of cataract and AMD. A review with his Ophthalmologist was also recommended, to keep close scrutiny of his level of distance vision for driving.
Case Study #2
Mrs E is a 91 year-old lady with a diagnosis of ‘legal blindness’ from Wet Age Related Macular Degeneration. Mrs E has enjoyed an active life, reading music, writing newsletters for a local community group and researching family history. her vision loss over the last several years had started to make these tasks impossible, causing her to feel depressed.
‘Legal blindness’ can be defined as being unable to see the top letter on a standard distance acuity chart with your best prescription (‘less than 6/60’) or ‘tunnel vision’ to the extent that ten degree or less is remaining in the better eye. Some people are defined as ‘legally blind’ when they have a combination of severe patchy field loss and poor distance acuity, making the combined effect a large burden on their daily life.
In Mrs E’s case, she contacted our Orthoptist, to help her explore aids so she can independently read music, despite having severe central vision loss. She had received other types of assistance in the past, such as white cane training and occupational therapy, at another agency for low vision.
The goal in seeing our Orthoptist was to explore a combination of ‘eccentric viewing training’ and electronic magnification to overcome the challenges she had started to face.
‘Mrs E’ also continued to receive injections for her Wet AMD from her Ophthalmologist (eye doctor).
During the initial Orthoptic assessment, the following was found:
Visual Acuity:
Right 1/36 Left 1/60 (Unable to see the distance chart at 6 metres, so the chart was brought closer, until, at one metre’s distance, Mrs E saw some letter. The finding indicate that she needed to be one metre away to see what the ‘normal eye sees at 36 metres distance. This is severe vision impairment, caused by her Macular Degeneration.
As Mrs E cannot see the top of the standard distance vision chart at 6 metres, this makes her vision fall into the classification of ‘legal blindness’.
Entitlements in line with the blind pension and travel were discussed.
Near vision was N80 or 80point (4 times larger than ‘large print’ book font). Mrs E could only read one letter at a time.
Glasses did not improve her distance or near vision.
See the photographs below depicting how she saw things like her garden and her reported view through a typical optical magnifier…

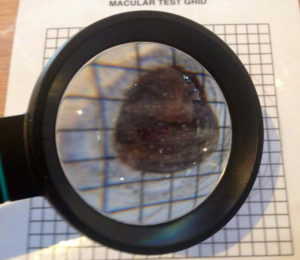
Looking through standard optical magnifiers only highlighted her central vision loss.
Electronic low vision aids offer more magnification, with a relatively generous field of view, which is particularly useful for Mrs E.
Mrs E demonstrated trouble reading words completely and finding her way when reading a sentence or page of print. This was with or without aids.
Despite already owning a small portable electronic magnifier (CCTV) Mrs E appreciated other CCTVs of a higher image definition.
Although these allowed her to see fine print, she still lost her place due to the large central scotoma (missing area) in her vision.
Mrs E therefore also explored CCTVs with margins to help reduce visual clutter.
Mrs E had her central fields mapped by the Orthoptist and it was shown that the closest remaining area of vision to the ‘straight-ahead’ viewing position was just below the centre. Therefore Mrs E started learning to look just above words a few degrees to bring this useful area of field into view.
With at least several sessions of training, patients generally learn to read font of diminishing size.
At the commencement of training, Mrs E struggled to read 80 point (print four times the size of ‘Iarge print’). She now reads font a quarter of this size and soon will be mastering standard magazine sized print.
We are currently continuing to meet with Mrs E to supply her with some “more challenging” font sizes and word combinations.
Whilst the macular is still affected and injections continue to help the overall management of her condition, Mrs E has learned to use her remaining vision to her best ability and can now appreciate the aids she uses to magnify words just a little more.
Eccentric Viewing is an established technique of Low Vision Rehabilitation which is based on scientific principles of the visual system.
Establishing whether or not you are suited to Eccentric Viewing Training is the role of the Low Vision Rehabilitation Orthoptist.
Well done, Mrs E!
Case Study #3
Bob is a 50 year-old male who had suffered a stroke twelve months prior to presenting for a Low Vision Assessment.
Bob’s eye doctor: (Ophthalmologist) has diagnosed him with: right sided bilateral homonymous hemianopia (half-field loss in each eye on right side) directly related to his left-sided brain injury from a stroke.

His doctor mentioned the issues which Bob has with his mobility, due to this un-resolvable loss in the right half of each eye’s visual field. He has had assistance from Guide Dogs Victoria for this problem, with the recommendation that he uses a white cane to assist his mobility. The field loss meets mid-line of vision, so Bob is unable to read sentences.
A Bob was under the age of 65, he was assessed by our Orthoptist through his funded hours provided by the National Disability Insurance Scheme.(NDIS)
Bob has stipulated he has the following goals.
GOAL 1) To be able to study a Certificate 2 in Horticulture (through local T.A.F.E. facility), despite significant vision loss related to his stroke and functional vision problems relating to his acquired brain injury.
For Goal 1, the aim of exploring electronic versus optical aids was pursued.
GOAL 2) To be able to read recipes at home despite significant visual field loss (side vision loss). Bob has stated that he lives alone since his wife passed away, so is responsible for cooking. He must cook healthy meals to be able to maintain his blood sugar levels. Traditional optical magnifiers explored in the past are no longer useful to him, as his vision has deteriorated further especially in the last 3 months.
To address Goal 2, the strategy of exploring adaptive technology was pursued.
Visual Fatigue is experienced by Bob, particularly with reading and using the computer. He finds it very difficult to maintain focus at all and struggles with reading complete words or short sentences.
OTHER HEALTH CONDITION(S) RELEVANT TO VISUAL FUNCTIONING
Diabetes
Bob has also been diagnosed with Diabetes. Diabetic Retinopathy has not currently been diagnosed, but is very much a possible complication of having Diabetes over many years, so there is the likelihood that Bob may suffer with further vision loss in the future, despite well controlled blood sugar levels.
Due to the likelihood of further vision loss due to Diabetes, it is recommended Bob’s CCTV have the feature of text to audio output as something that may be added if necessary. The link below provides a brief outline of diabetic retinopathy ad how it impacts on vision, due to damage to the retinal blood vessels.
Acquired/Traumatic Brain Injury (post stroke)
Those with acquired and/ or traumatic brain injury (A/TBI) have a much higher incidence of binocular vision dysfunction and accommodative (focusing) disorders as well as issues of balance and a host of perceptual anomalies including a shifted concept of mid-line.
VISION FINDINGS from Orthoptic assessment
Distance Vision: (Uncorrected) Right eye 6/36 Left eye 6/24 part.
This means: what the normal eye sees at 24-36 metre’s distance: Bob can only see, if standing at a 6m distance from the same sized object. Distance vision did not improve significantly using the ‘pinhole test’. This confirms that Bob’s distance acuity is un-correctable with prescription glasses.
The combination of reduced fields in each eye and reduced distance and near acuity make Bob vision impaired, thus requiring adaptive technology to allow him to see for near and far.
Near vision:
(with reading glasses) N14-18 BEO (preferring large print N20: as used in large print books) for comfort. Bob has reduced near vision despite wearing a recent glasses prescription.
Prefers this size print.
Range of accommodation: (range of focus)
Bob has a limited range of accommodation, which, in combination with the above vision loss and his ABI, explains why he experiences visual fatigue after very short periods or reading and would benefit from an electronic rather than a traditional optical magnification device.
EYE MOVEMENTS
There was no squint or indication of any tendency for the eyes to drift inwards or outwards when Bob’s eye movements and co-ordination were briefly examined.
The reduced range of accommodation, however, will lead to easy visual fatigue, hence enforcing the need for an electronic rather than optical magnifier, as an electronic magnifier (CCTV) can be used at a further distance from the eyes, suiting his limited range of accommodation.
OUTCOMES
Bob has explored a range of both optical and electronic magnification devices to relieve his visual fatigue. Optical magnifiers only enhanced the visual discomfort he experiences with closely positioned objects, as (due to the narrower field of view) he must move the magnifier a lot and still failed to see all parts of a word on a page.
It was therefore recommended that a larger CCTV in additional to extra scanning training were the most appropriate solutions for Bob’s situation. Both of these recommendations were approved through NDIA, following a detailed Orthoptic Specialist Assessment Vision Report.